Party Drug Tested as PTSD Cure
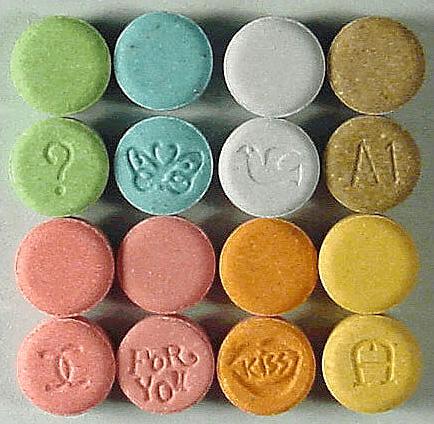
Tablets containing MDMA. Credit: Wikipedia
The Food and Drug Administration has approved party drug MDMA, also known as Ecstasy, to be trialed in a large-scale study as a cure for severe Post-Traumatic Stress Disorder. The study received the green light on November 29th with the possibility of prescription drug distribution in 2021.
The approval is not without concern, according to Duncan Laird, Williston’s director of psychological counseling services. “There needs to be a lot of really well-controlled, good scientific research about the use of MDMA for therapeutic purposes,” he said. “If they are well researched and there is psychotherapy along with the administration of medication, then I think that is worth researching to see if it can be helpful.”
MDMA is a synthetic drug that produces feelings of increased energy, pleasure, emotional warmth, and distorted sensory and time perception, according to the National Institute on Drug Abuse. It was originally researched as a possible drug for anxiety in the 1970s, but it became an illegal street drug.
Prior small-scale studies consisted of 12 weeks of psychotherapy, including three eight-hour sessions where the patients took the drug. By the end of one of the studies, two-thirds of the patients no longer met the criteria for PTSD.
Laird said PTSD can cause both a mental and physical reaction.
“The early warning system in the brain is on hyper alert and it is responding to stimuli in people’s everyday environment that is inappropriate for the brain to respond to,” he said. “But the brain has been in this hyper alert mode and so people are going into high states of acute anxiety and their bodies are also doing that.”
MDMA allows patients feel comfortable and happy discussing their trauma. Patients who have no luck with other forms of therapy or medication are finding success. Most patients are veterans or rape victims, and have been struggling with PTSD for an average of seventeen years, according to a November 29 New York Times article.
The MDMA, combined with the psychotherapy sessions, have helped several PTSD sufferers. In a New York Times, article, C.J. Hardin said the drug changed his life.
“It allowed me to see my trauma without fear or hesitation and finally process things and move forward.” Hardin toured in Iraq and Afghanistan and could not find any cure for his PTSD after his service. He was alcoholic, suicidal, living as a hermit in a cabin, and had given up on finding a cure.
Despite mostly positive results, there are doubts and concerns about using the drug as a cure for PTSD. Legalizing the drug as a prescription could lead to more recreational use and abuse. There is the possibility of a psychedelic crisis (a bad trip); this risk is amplified for people with mental illness, according to the non-profit Drugs Forum website. Also, prolonged use of Ecstasy can lead to brain damage.
Mr. Laird worries the approval of MDMA as a prescription drug could have the same fate as opioids, such as OxyContin, Vicodin, or Fentanyl. These drugs are highly addictive and destructive, and the United States is in the midst of an opioid overdose epidemic. “I don’t think we know enough to know if there is going to be a rebound,” Laird commented.
Williston student Kevin O’Sullivan ’18 said, “I believe that if it is truly proven to be an effective treatment for PTSD then it should most certainly be a prescribed medication. In some cases, I know that medicinal marijuana has been very useful, like for people with Parkinson’s disease.” However, O’Sullivan disagrees with the FDA process of human testing. “I don’t believe they should be testing these drugs on people, even if they give their consent, because it can be dangerous.”
Similar to MDMA testing, another study prescribes psilocybin to cancer patients to help reduce their anxiety and depression. Psilocybin is an psychedelic compound produced by some strains of mushrooms. Laird believes there will be more testing and research on the use of these types of drugs for medicinal purposes in the future.
“There is going to be a shift in the willingness of both the FDA to use well-researched new drugs that have historically been used for recreational purposes to be available to people, especially for psychological distress, such as end of life care, people who are experiencing severe moments of depression, PTSD, anxiety, [and] people who have a terminal illness,” said Laird. “I do think we will see an acceptance and an approval, especially as the baby boomer generation gets older. Whether it is 2017 or 2025, I think it is going to happen.”
Sophia is a six-year senior from Northampton, MA. She likes to play lacrosse and talk to her sister in a funny voice.